A Comprehensive Guide to the 5 Stages of Dementia: Signs, Progression, & Treatment

- What is Dementia?
- Dementia Stages: What They Mean and Where They Came From
- What are the 5 Stages of Dementia
- What are the Different Types of Dementia?
- Diagnosing and Identifying Dementia Stage
- Treatment and Care for People with Dementia
- FAQs
If you’re looking for your car keys (again) or can’t remember why you just walked into the kitchen (again), you may joke and secretly worry that you have dementia. Don’t worry; distraction, disorganization, and even forgetfulness do not represent dementia. There is much more to it than typical absent-mindedness due to aging or too much going on.
Similarly, an aging parent, a spouse or other loved one may show signs of cognitive decline. But before assuming they suffer from dementia, learn more about the condition by exploring the different stages of dementia, their symptoms, progression, and strategies for managing the condition.
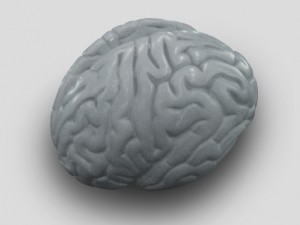
What is Dementia?
Dementia is a complex condition that interferes with a loved one’s memory, communication, language, judgment, and overall brain function. Dissimilar from memory slips that can occur with old age, dementia is a progressive malady that can be caused by Alzheimer’s disease, and it impairs parts of the brain that are vital in processing speech and spatial awareness. It is very common for people to confuse dementia with old age. After all, it’s normal for people to forget things as they get older; however, dementia and age-related memory loss are two entirely different things.
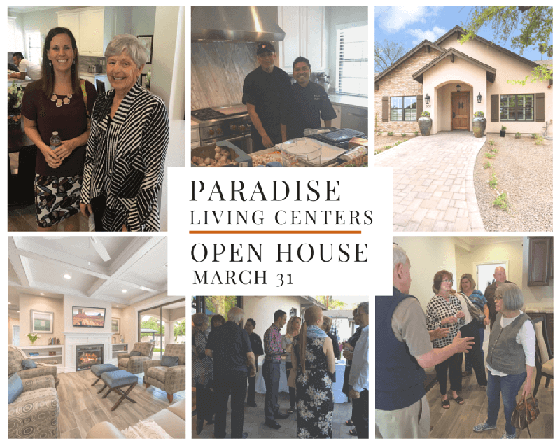
While it may be frustrating to watch your loved one struggle with dementia, this should be the time to consider professional care from highly trained specialists. At Paradise Living Centers, residents with dementia receive around-the-clock care from our certified caregivers and licensed nurse. It’s our mission to ensure residents are given the quality care they deserve, and their families are given the peace of mind they desire.
Dementia Stages: What They Mean and Where They Came From
Healthcare providers use a scale to evaluate the stage and progression of dementia. The exact number of stages may differ depending on which scale is used, but generally, the higher the stage, the more severe the cognitive decline. For example, stage one would be no symptoms of dementia, while stage 3 would be moderate dementia symptoms and so on.
One of the most common measures of dementia is the Reisberg or Global Deterioration Scale (GDS). It breaks down the progression of dementia into seven stages. Another commonly used measure, the Clinical Dementia Rating Scale (CDR), is discussed further in the next section. Experts originally developed these scales for patients with Alzheimer’s disease, but they can be used for staging non-Alzheimer’s disease dementia as well.
What are the 5 Stages of Dementia?
The CDR Scale categorizes dementia into five different stages. Each stage of these rating scales assesses the severity of symptoms in different categories, including memory, orientation, judgment and problem-solving, community affairs involvement, home life, hobbies and personal care.
At Paradise Living Centers, we want to take a moment to educate family members about the five stages of dementia. If you believe your loved one is suffering from dementia, learning about these five stages will help you provide appropriate care and support to individuals living with the condition.
Stage 1: CDR-0, No Impairment
Patients with a CDR score of 0 generally show no signs of impairment or memory loss that interfere with their normal abilities. This means your loved one has no significant memory problems, and they are able to take care of their personal needs without the help of others.
During this stage, individuals may experience typical age-related memory lapses, but these do not significantly impact their overall cognitive abilities. It’s important to note that not all individuals progress through the stages of dementia at the same pace, and some may remain in Stage 1 for an extended period.
Stage 2: CDR-0.5, Questionable Impairment
This score demonstrates very slight impairments in cognitive function. This stage usually resembles minor memory loss, but virtually no issues with personal care. If your loved one suffers from Stage 2 dementia, they may have difficulty solving problems or timing things.
The presence of questionable impairment suggests a subtle decline in cognitive abilities compared to Stage 1. Memory lapses may become more noticeable, and individuals might struggle to remember recent events or retain new information.
Stage 3: CDR-1, Mild Impairment
Stage 3 dementia can disrupt your loved one’s ability to perform normal activities outside the home. If they have trouble with directions or begin neglecting personal chores, you may want to have them see a specialist for care.
The mild impairment seen in Stage 3 suggests a noticeable decline in cognitive abilities compared to earlier stages. Individuals may have trouble remembering recent events, experience confusion with time and place, and exhibit difficulties in judgment and problem-solving. While they may still manage basic self-care tasks, their ability to handle complex activities and navigate unfamiliar environments may be compromised.
Stage 4: CDR-2, Moderate Impairment
Patients with stage 4 dementia struggle with personal hygiene, daily chores, and social activities. At this point, your loved one’s short-term memory is seriously impaired, which means they may have trouble remembering new people.
In Stage 4, the decline in cognitive abilities becomes more pronounced, impacting various aspects of daily life. Individuals may struggle with maintaining personal hygiene, such as bathing, grooming, and dressing themselves. They may require assistance or reminders to perform basic tasks. They may also rely heavily on established routines and familiar surroundings to compensate for their memory deficits.
Stage 5: CDR-3, Severe Impairment
A CDR-3 score indicates Stage 5 or severe dementia, which means your loved one cannot function without the help of a caregiver. The understanding of time, direction, and taking care of one’s personal needs are completely gone at this point in time.
Stage 5 is considered late-stage, severe dementia. People at this stage, particularly those stricken with Alzheimer’s disease, will have severe memory loss along with reasoning difficulties. They will no longer be able to speak or communicate coherently and may exhibit some really strange behavior. They cannot eat, dress, or use the bathroom without help.
Physically, they may no longer be able to walk or even hold their head up without support. Muscles become rigid, and eventually, their ability to swallow or control bodily functions fails. Comparatively, this would be stage 7 on the GDS scale.
What are the Different Types of Dementia?
There are several different types of dementia, each characterized by unique causes, symptoms, and progression.
This accounts for the majority of cases. It is characterized by the accumulation of amyloid plaques and tau tangles in the brain, leading to progressive cognitive decline, memory loss, and changes in behavior.
This is caused by reduced blood flow to the brain, often due to stroke or other vascular conditions. Symptoms may include problems with thinking, memory and difficulty with movement and coordination.
-
Lewy Body Dementia
This is characterized by the presence of abnormal protein deposits called Lewy bodies in the brain. It can cause various symptoms, including fluctuations in alertness, visual hallucinations, movement difficulties, and cognitive impairments similar to Alzheimer’s.
-
Frontotemporal Dementia
Frontotemporal dementia primarily affects the frontal and temporal lobes of the brain. It leads to changes in personality, behavior, and language skills. Memory loss may be less prominent in the early stages than other types.
-
Parkinson’s Disease Dementia
People with Parkinson’s disease may develop dementia as the disease progresses. Symptoms include movement difficulties, tremors, and cognitive changes such as memory loss, slow thinking, and impaired judgment.
-
Mixed Dementia
Mixed dementia refers to a combination of two or more types, most commonly Alzheimer’s disease and vascular dementia. It presents a mix of symptoms associated with the different types involved.
-
Other Types
There are rarer dementia types, such as Creutzfeldt-Jakob disease, Huntington’s disease, and Wernicke-Korsakoff syndrome, associated with specific underlying causes or conditions.
It’s important to note that each type has its unique characteristics, and accurate diagnosis is crucial for appropriate management and care.
Diagnosing and Identifying Dementia Stage
Accurate diagnosis and stage identification are essential for developing an appropriate care plan as the disease progresses. Diagnosing dementia involves a comprehensive evaluation that includes medical history, physical examination, cognitive tests, and sometimes imaging scans.
The healthcare professional will assess the individual’s symptoms, cognitive abilities, and functional impairments to determine the stage of a person’s dementia.
In addition to medical assessments, healthcare professionals may also consider input from family members or caregivers who have observed the individual’s behavior and cognitive changes over time. The combination of clinical evaluations, cognitive testing, and imaging results can help accurately diagnose and determine the stage of dementia.
Once a dementia diagnosis is established, the healthcare team can provide information and support to the individual and their loved ones, helping them understand the progression of the disease and plan for future care needs.
Treatment and Care for People with Dementia
There are no long-term treatments for dementia. As of yet, nothing is available that will slow the progression or provide a cure, but there are steps that families and care providers can take to improve the situation in the short run.
These treatments and interventions aim to manage symptoms, slow the progression, and improve the overall quality of life of people with dementia, often involving a combination of medications, therapies, and supportive care.
Medications and Therapies
Depending on the type and stage of dementia, healthcare providers may prescribe medications to manage cognitive symptoms, such as memory loss and confusion.
Additionally, non-pharmacological therapies can complement medication treatments. Cognitive stimulation programs, reminiscence therapy, and music or art therapy can enhance cognitive abilities, reduce anxiety, and promote social engagement.
Supportive Care
Creating a supportive and safe environment is essential for individuals with dementia. Caregivers and family members can modify the home environment to reduce falls and accidents and enhance independence. This may include installing grab bars, removing trip hazards, or labeling commonly used items.
Paradise Living Centers enlists memory care experts to work with our residents and lead them in activities that engage and help slow down cognitive decline.
Lifestyle Changes
Maintaining a structured routine and engaging in regular physical exercise can also contribute to overall well-being. Physical activity helps maintain physical function, promotes better sleep patterns, and reduces behavioral symptoms.
A healthy diet of fruits, vegetables, whole grains, lean proteins, and proper hydration supports overall brain health. Avoiding excessive alcohol consumption and quitting smoking can also have a positive impact.
Dementia may be difficult to deal with, but it doesn’t have to turn life upside down for you and your family.
Call Paradise Living Centers in Paradise Valley and Phoenix to speak to our Care Manager about our memory care program and other care services. We are here to help. Call 480.878.4112 today!
FAQs
Is dementia hereditary?
Some forms of dementia have a genetic component, meaning they can run in families. However, not all cases of dementia are hereditary, and having a family member with dementia does not guarantee that an individual will develop the condition.
Can dementia be prevented?
While there is no surefire way to prevent dementia, certain lifestyle choices may help reduce the risk. These include engaging in regular physical exercise, maintaining a healthy diet, staying mentally and socially active, managing chronic conditions, and avoiding smoking and excessive alcohol consumption.
What are the early signs and symptoms of dementia?
The early signs of dementia can vary depending on the specific type and individual, but there are some common symptoms to be aware of. These signs may develop gradually and often go unnoticed in the earlier stages of the disease.
Dementia symptoms typically include:
-
Memory Loss
Difficulty remembering recent events or important information is often one of the earliest signs of dementia. Individuals may forget appointments, conversations, or where they placed objects.
-
Confusion and Disorientation
People with early-stage dementia may experience confusion and have trouble following directions or finding their way in familiar environments.
-
Language Difficulties
Struggling to find the right words, forgetting familiar words, or having difficulty understanding and following conversations are common language-related challenges in the early stages of dementia.
How does dementia progress?
Dementia is a progressive condition, meaning symptoms tend to worsen over time. The rate of progression can vary from person to person and depends on the underlying cause of dementia. As the condition progresses, individuals may experience the following changes:
-
Increased Memory Loss
Memory problems become more pronounced, affecting both short-term and long-term memory. Individuals may struggle to recognize familiar faces or places.
-
Communication Challenges
Language difficulties become more apparent, with individuals having difficulty following or participating in conversations. They may also struggle with reading and writing.
-
Behavioral and Mood Changes
Personality changes and mood swings can occur as dementia progresses. Individuals may become irritable, anxious, or even exhibit aggressive behavior. They may also experience depression and withdrawal from social activities.
What is the difference between dementia and Alzheimer’s disease?
Dementia is a general term that refers to a decline in cognitive function, while Alzheimer’s is a specific type of dementia. It is characterized by the buildup of abnormal protein plaques and tangles in the brain, leading to progressive cognitive decline.
What are the stages of memory loss in dementia patients?
Memory loss is a hallmark symptom of dementia, and it can progress through different stages as the condition worsens. The stages of memory loss in dementia include:
-
Early Stage
In the early stages, individuals may experience occasional forgetfulness and difficulty remembering recent events or conversations.
-
Middle Stage
Memory loss becomes more pronounced in the middle stages of dementia. Individuals may struggle to recall important details, such as names, dates, or significant life events.
-
Late Stage
Severe memory loss characterizes the end stages of dementia. Individuals may struggle to recognize close family members and have difficulty recalling personal information or memories from their past.
How long does dementia last?
The duration of dementia can vary widely depending on several factors, including the type of dementia, individual health, and access to appropriate care.
On average, individuals live with dementia for approximately 8 to 10 years after the initial diagnosis. However, the disease’s progression is highly individualized, and some individuals may live with dementia for a shorter or longer period.
What stage of dementia is repetition?
Repetition is a common behavior in individuals with dementia and can occur in different stages of the condition. However, it is often more prevalent in the middle and late stages of dementia. As cognitive function declines, individuals may repeat questions, statements, or actions due to memory deficits and difficulty retaining new information.
At what stage do dementia patients forget family members?
Forgetting family members can occur at different stages of dementia, but it is typically more prevalent in the later stages. As the condition progresses, individuals may struggle to recognize and remember close family members, including spouses, children, or siblings. However, it’s important to note that the rate and extent of memory loss can vary among individuals.
What stage of dementia is sundowning?
Sundowning, also known as late-day confusion, is commonly associated with the middle and late stages of dementia. It refers to a pattern of increased confusion, agitation, and restlessness that tends to occur later in the day or evening. While sundowning can vary in severity and frequency, it is more prevalent in the middle and later stages of dementia.
What is “end stage” dementia?
The term “end stage” is often used to describe the late stages of dementia when individuals experience a significant cognitive and physical decline. In this stage, individuals typically require round-the-clock care and assistance with all activities of daily living. However, it’s important to note that the specific staging terminology can vary depending on the assessment tool or framework healthcare professionals use.
What can we do for people with late-stage dementia?
Although research has yet to yield something new on the medicinal front, that doesn’t mean the care of people with severe dementia should solely be focused on their physical needs. Care should provide comfort, preserve dignity and include activities that stimulate the senses.
Experts recommend focusing on small repetitive tasks that engage each of the senses: sight, touch, smell, hearing and taste. However, always consult with the clinical staff before running any activities, and arm yourself with realistic expectations.
Conclusion
Early diagnosis and intervention are crucial in dementia management. If you suspect your loved one may be experiencing cognitive decline, it is recommended to seek a comprehensive evaluation from healthcare professionals who specialize in dementia care. They can provide a more accurate diagnosis, offer guidance on treatment options, and provide support for both the individual and their caregivers.
If you have any questions about how to best care for someone diagnosed with dementia or our assisted living community, please contact Paradise Living Centers at (480) 878-4112.


 Wednesday, May 25th is National Seniors Fitness and Health Day and approximately 100,000 older adults will participate in activities at more than 1,000 locations throughout the U.S. This year’s theme is “Improve Your Health for a Better Self,” which encourages older Americans to get healthy and fit and focus on becoming the best they can be.
Wednesday, May 25th is National Seniors Fitness and Health Day and approximately 100,000 older adults will participate in activities at more than 1,000 locations throughout the U.S. This year’s theme is “Improve Your Health for a Better Self,” which encourages older Americans to get healthy and fit and focus on becoming the best they can be.